While the holidays are traditionally a time of togetherness and joy with family and friends, it can be hard to find the joy – and the endurance to get through them – while grieving.
Eleanor Haley of What’s Your Grief offers the following Seven Ways to Go Easy on Yourself While Grieving at the Holidays:
1. Remember, the Holidays Don’t Have to Be Perfect.
Disavow yourself of the notion that perfection will protect you from experiencing grief and sadness this holiday season. Spoiler: It: won’t. No matter how tender you cook your brisket or how elegantly you set your holiday table, someone is missing… and this devastating reality is a constant.
Also, you don’t have to be perfect to prove anything to anyone else. People commonly feel they have to put on a brave face to convince others they are doing well, but it’s especially common to struggle with grief this time of year—regardless of how long ago your loss occurred. So if you’re off your holiday-game, you have a good excuse. Own it.
In the end, “perfection” is way overrated anyway. As we wrote in our article, New Perspectives on Old Traditions:
“In reflecting on holidays past what’s more likely to make you smile – the holiday when you had spaghetti for dinner because the dog ate the roast or the year everything went as planned? When it comes to family, imperfection is perfection. Working together to get through the holidays despite inescapable flaws will help deepen family bonds and create a supportive environment for grief and remembrance.”
2. Be Intentional but Flexible About Tradition.
Tradition is incredibly important, so it’s a tender spot for many grieving people. Tradition provides a sense of comfort and security. It’s a tie that binds the past to the present, and it bonds people on Earth to those they love who have died. But after a death, it’s usually something that has to change.
Breaking tradition feels like succumbing to yet another loss, so there’s often resistance around making changes. Many try to keep everything the same, but this often makes the loved one’s absence even more glaring because the only difference is that they aren’t there.
An important question to ask as a family is: How do we honor tradition while also allowing it to change? For every family, the answer will be different, but one place to start is to focus on why you participate in the tradition in the first place.
Consider: What is the value at the heart of your ritual? Togetherness, generosity, shared history, spirituality? Quite often, you’ll find that it’s okay for some of the ‘what’ to change, so long as you still connect with the “why.”
3. Practice Saying “No.”
From November to January, commitments, pressures, and stressors tend to increase for everyone. As someone who is grieving, you have the added challenge of dealing with loss and change, which means you have less physical, emotional, and mental energy to go around.
If you know you are someone who says ‘yes; to every invitation and request, you may want to try and say ‘no’ a little more these next few weeks. We’re not suggesting you opt-out of everything, but rather you prioritize the most important commitments over the activities and events you probably won’t mind missing.
Resist the temptation to stay busy or to say “I’m fine” and brush your grief aside. Be honest with yourself (and others) that things are a little different this year. In order to take good care of yourself and those you care about, you may need to take it easy—and that’s okay!
4. Schedule “Me” Time.
So, now that you’re saying ‘NO’ more judiciously, we want you to re-invest some of that time in your own well-being. Work specific coping activities into your weekly calendar and plan for time-outs during busy activities and gatherings.
5. Utilize Your Resources and Ask for Help.
You’re not alone in this (though we know it may sometimes feel like you are). Even if you don’t have family and friends you can count on, there are services and groups in your community that can hopefully help you make it through.
If you aren’t sure what help you need, try our article Thanks for the Offer, But I Don’t Know What I Need. If you know what you need but aren’t sure how to ask for help, try Helping Your Friends Help You. And if you have no time for subtly, just send your support system the article 8 Tips for Supporting a Grieving Friend This Holiday.
6. Allow Yourself To Experience Moments of Comfort and Joy.
First of all, please know that whatever you’re feeling right now is okay. Experiencing positive emotions during the holidays is never a given, especially when you’re grieving. All we’re saying is that if you do surprise yourself by laughing at Buddy the Elf or smiling at the grandkids unabashed joy on Christmas morning, go with it and don’t feel guilty.
Experiencing things like okay-ness, comfort, happiness, gratitude, and joy can feel like a betrayal to deceased loved ones—but it’s not. And I don’t say this because I simply know your loved one would want you to be happy (I have no way of knowing that, though I’m sure they would). Rather I say this because emotions are not either-or and you can feel far more than one thing at a time. Things like laughter and warmth, for example, don’t cancel out your sadness.
7. Find Opportunities To Connect With Your Loved One.
One of the best ways to cope with the pain of missing a loved one at the holidays is to find ways to connect with them and to incorporate their memory into your holiday gatherings and celebrations.
Though it can feel isolating when others don’t want to recognize the loss in the same way you do, try not to feel too discouraged if those you plan to spend the holidays with aren’t open to connecting with your loved one in the same way you are. Studies show that private rituals can be just as, if not more, healing than larger remembrances.






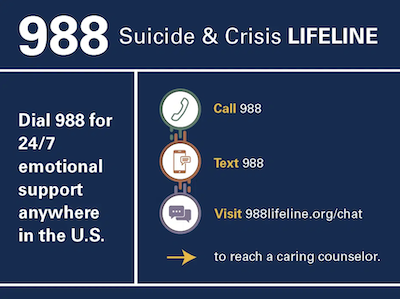
 Ernst started working with Provident Behavioral Health, working with the suicide crisis line and the Hope After program, a case management program for people who may have been hospitalized with suicidal ideation. At the same time, she was also doing hospice work.
Ernst started working with Provident Behavioral Health, working with the suicide crisis line and the Hope After program, a case management program for people who may have been hospitalized with suicidal ideation. At the same time, she was also doing hospice work.
 The increase could be fueled in part by the loss, isolation and life disruption of the Covid-19 pandemic, but Kristen Ernst MA, LPC owner of the Center for Hope and Healing, LLC, in St. Charles, Mo., says there are also other factors at play.
The increase could be fueled in part by the loss, isolation and life disruption of the Covid-19 pandemic, but Kristen Ernst MA, LPC owner of the Center for Hope and Healing, LLC, in St. Charles, Mo., says there are also other factors at play. 


 He was very serene baby. Never a problem. He had beautiful blonde curly hair. I do childcare in my home. So he grew up with all ages of children played with kids every day. When he went to school I remember the first two weeks he cried and cried. He did not want to get on that bus. I don’t know if I traumatized him. I think back and I’m like, Oh my God, is that why? I’m like, Why did I make him do that? I should have went with him. He was very, very sensitive. Like, if you even reprimanded him when he was little, he would just get so teary eyed, even if he didn’t really do anything wrong. That’s how sensitive he was.
He was very serene baby. Never a problem. He had beautiful blonde curly hair. I do childcare in my home. So he grew up with all ages of children played with kids every day. When he went to school I remember the first two weeks he cried and cried. He did not want to get on that bus. I don’t know if I traumatized him. I think back and I’m like, Oh my God, is that why? I’m like, Why did I make him do that? I should have went with him. He was very, very sensitive. Like, if you even reprimanded him when he was little, he would just get so teary eyed, even if he didn’t really do anything wrong. That’s how sensitive he was.